Beyond Home Visits: How Healthcare Reforms Reduced Child Mortality in Rural Mali
A study in rural Mali found that proactive home visits by community health workers did not significantly reduce under-five mortality compared to fixed-site care. However, broader system-strengthening measures, such as removing user fees and improving healthcare infrastructure, contributed to a notable decline in child mortality in both groups.
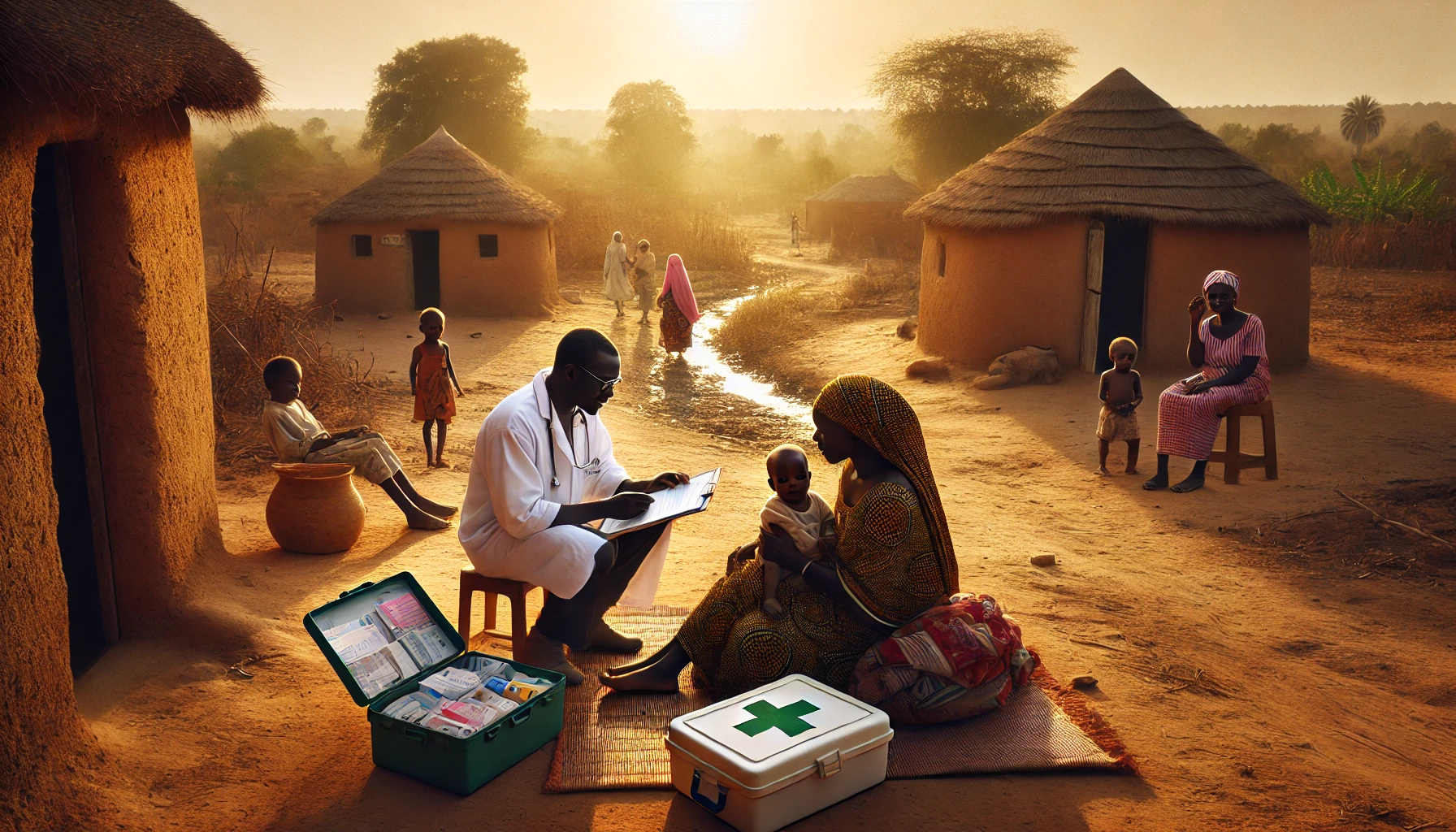
A study published in the Bulletin of the World Health Organization examined the effect of proactive home visits by community health workers (CHWs) on child survival rates in rural Mali. The trial was conducted from 2017 to 2020, testing whether home visits could reduce under-five mortality compared to services provided by CHWs at fixed healthcare sites. The randomized controlled trial involved 137 village clusters, and more than 31,000 children were enrolled at the start or during the study. Mali, particularly in rural areas, has long struggled with high under-five mortality rates, partly due to barriers such as user fees, long distances to health facilities, and a shortage of trained healthcare workers. These issues often prevent timely access to healthcare, exacerbating morbidity and mortality in children. To address these challenges, the study aimed to evaluate if home visits, where CHWs proactively provide healthcare services to families in their homes, could bridge gaps in healthcare access, especially in remote areas.
The Impact of CHW Home Visits on Child Mortality
In the trial, the intervention arm received proactive case detection services through regular home visits by trained CHWs, while the control arm relied on CHWs delivering healthcare from fixed community sites. To improve the overall quality of care, the study also implemented several system-strengthening measures in both arms, including the removal of user fees, improvements to staffing, and infrastructure upgrades at local primary healthcare centers. These changes were aimed at eliminating the financial and logistical barriers that often prevent families from seeking timely medical attention for their children.
Significant Reductions in Mortality Across Both Study Groups
Over the three years of the study, more than 52,000 person-years of observation were recorded. By the end of the trial, 909 children had died in the intervention arm, compared to 827 in the control arm. The under-five mortality rate saw a sharp decline in both groups. In the intervention arm, the mortality rate decreased from 142.8 deaths per 1,000 live births to 56.7, while in the control arm, it fell from 154.3 to 54.9. Despite these impressive reductions, the analysis showed no significant difference between the intervention and control groups in terms of mortality reduction. The intention-to-treat analysis, which included all participants as assigned to their respective study arms, indicated an incidence rate ratio (IRR) of 1.02, with a 95% confidence interval of 0.88 to 1.19, suggesting that home visits did not provide a statistically meaningful advantage over fixed-site care. Similarly, the per-protocol analysis, which only considered participants who adhered strictly to the study protocol, also found no significant difference, with an IRR of 1.01.
System-Level Reforms May Have Been Key to Success
These findings highlight an important conclusion: while proactive home visits did not yield additional benefits in reducing under-five mortality compared to fixed-site care, the overall decline in mortality across both groups was significant. This suggests that the broader system-strengthening measures, such as the removal of user fees and improved healthcare infrastructure, likely played a pivotal role in the reduction of child mortality. The presence of trained CHWs in communities, regardless of whether they delivered care through home visits or at fixed sites, may have been a more critical factor in improving access to healthcare and ultimately saving lives. The findings challenge the assumption that home visits alone are a key driver of better health outcomes and indicate that other factors, such as the accessibility and quality of healthcare services, may be more impactful.
Health System Strengthening in Conflict Zones
The trial took place in a region of Mali that faced significant challenges, including poverty, limited healthcare access, and ongoing armed conflict. These conditions often exacerbate child mortality rates, as conflict disrupts healthcare delivery and displaces families, making it harder to access services. Despite these challenges, the substantial drop in child mortality during the trial period is notable, particularly given the context of violence and instability in the region. The trial provides important evidence for policymakers in low- and middle-income countries who are seeking to improve child survival through community-based healthcare interventions. It suggests that while CHW home visits may not necessarily lead to further reductions in mortality, system-wide improvements, such as eliminating user fees and ensuring consistent healthcare provision, can have a powerful impact.
Lessons for Future CHW Service Organization
The study also raises questions about how best to organize CHW services in resource-limited settings. In this trial, the removal of fees and the strengthening of healthcare infrastructure appeared to be more important for reducing under-five mortality than the specific delivery method of CHW services. This finding is consistent with other research that suggests that the presence of trained healthcare workers in communities and the elimination of financial barriers can significantly improve health outcomes, particularly for children. Future analyses of the trial data may explore other factors, such as the spatial relationship between households and healthcare sites, and the dose-response effects of CHW services on child mortality, to better understand how these interventions can be optimized. Overall, the study underscores the need for holistic approaches to improving healthcare in low-resource settings and highlights the potential of system-level reforms to drive significant health gains for vulnerable populations.
- FIRST PUBLISHED IN:
- Devdiscourse
ALSO READ
Somalia Thwarts Major IS Attack in Puntland: A New Era of Conflict
Toward a Modern Land Market: Tackling Informality in Ukraine’s Agricultural Sector
Islamic State Escalates Military Attacks in Somalia's Puntland
Starry Nuptials: Armaan Malik Weds Fashion Influencer Aashna Shroff
Ethiopia and Somalia Revitalize Diplomatic Relations Amidst Regional Tensions










