WHO’s Comprehensive Approach to Preventing Rheumatic Fever and Heart Disease: A 2024 Roadmap
The WHO’s 2024 guideline on rheumatic fever and rheumatic heart disease focuses on prevention, early diagnosis, and management, emphasizing evidence-based interventions for high-risk populations. It highlights strategies like improved living conditions, antibiotic use, and early detection through diagnostic tools to reduce the global burden of these preventable diseases.
The World Health Organization (WHO) published a comprehensive guideline in 2024 focusing on the prevention and diagnosis of rheumatic fever (RF) and rheumatic heart disease (RHD), which was developed following a meticulous process involving extensive research and collaboration with a variety of experts and institutes. Researchers from WHO’s departments, including Maternal, Newborn, Child and Adolescent Health and Ageing, Noncommunicable Diseases, Antimicrobial Resistance, and Neglected Tropical Diseases, contributed to this effort. The guideline development was initiated in response to a resolution by the WHO Executive Board in 2017 that underscored the significant health burden posed by RF and RHD globally. The guideline aims to provide clear, evidence-based recommendations to address these preventable conditions, which remain a major public health issue in many low- and middle-income countries. The process of developing the guidelines followed WHO’s Handbook for Guideline Development, adhering to strict international standards for quality and transparency.
Defining Key Questions for Targeted Prevention
The guidelines were developed through a multi-step process, starting with the definition of the scope and the identification of key research questions. These questions guided the systematic reviews, which were conducted to assess the evidence available for the prevention, diagnosis, and management of RF and RHD. The focus was primarily on strategies to prevent the conditions from occurring and to identify them early, rather than on the later-stage management or treatment of advanced RHD, which is a topic planned for future guidelines. The WHO Steering Group, comprised of experts from various departments, played a key role in managing the development of the guideline, providing technical and procedural support, and ensuring that the work adhered to WHO’s policies. They also identified and approved members of the Guideline Development Group (GDG), a panel of external experts with diverse technical skills and backgrounds, ranging from clinical specialists to individuals with lived experiences of RF and RHD. The GDG was responsible for formulating the recommendations, reviewing the evidence, and finalizing the guideline document.
Systematic Reviews and Evidence-Based Recommendations
To support the guideline development, WHO contracted three systematic review teams through a competitive bidding process. These teams conducted reviews of the scientific literature, assessed the quality of evidence using the GRADE (Grading of Recommendations Assessment, Development and Evaluation) system, and presented their findings to the GDG. This evidence informed the key recommendations, which were formulated through consensus during virtual meetings held in 2021 and 2023. The systematic reviews focused on specific interventions aimed at reducing the incidence of RF and RHD. One of the primary areas of focus was primordial prevention, which addresses environmental and social factors that contribute to the spread of group A Streptococcus (GAS), the bacteria responsible for causing RF. The guideline emphasizes the importance of improving living conditions, reducing household crowding, and ensuring better access to healthcare in high-risk areas. Additionally, primary prevention strategies were highlighted, including the identification and treatment of streptococcal infections in children and adolescents to prevent the progression to RF and RHD.
Focus on Secondary Prevention to Avoid Recurrence
Another key component of the guideline is secondary prevention, which focuses on preventing recurrence of RF in individuals who have already experienced the disease. This includes the use of long-term antibiotic prophylaxis to reduce the risk of recurrent infections, which can lead to the development of RHD, a chronic condition that damages the heart valves. The guideline recommends specific antibiotics, such as penicillin, for both primary and secondary prevention, and outlines the appropriate dosages and administration methods. In areas where laboratory confirmation of streptococcal infections is not feasible, the guideline suggests clinical algorithms for diagnosing streptococcal pharyngitis and skin infections, enabling healthcare providers to make informed decisions about antibiotic treatment.
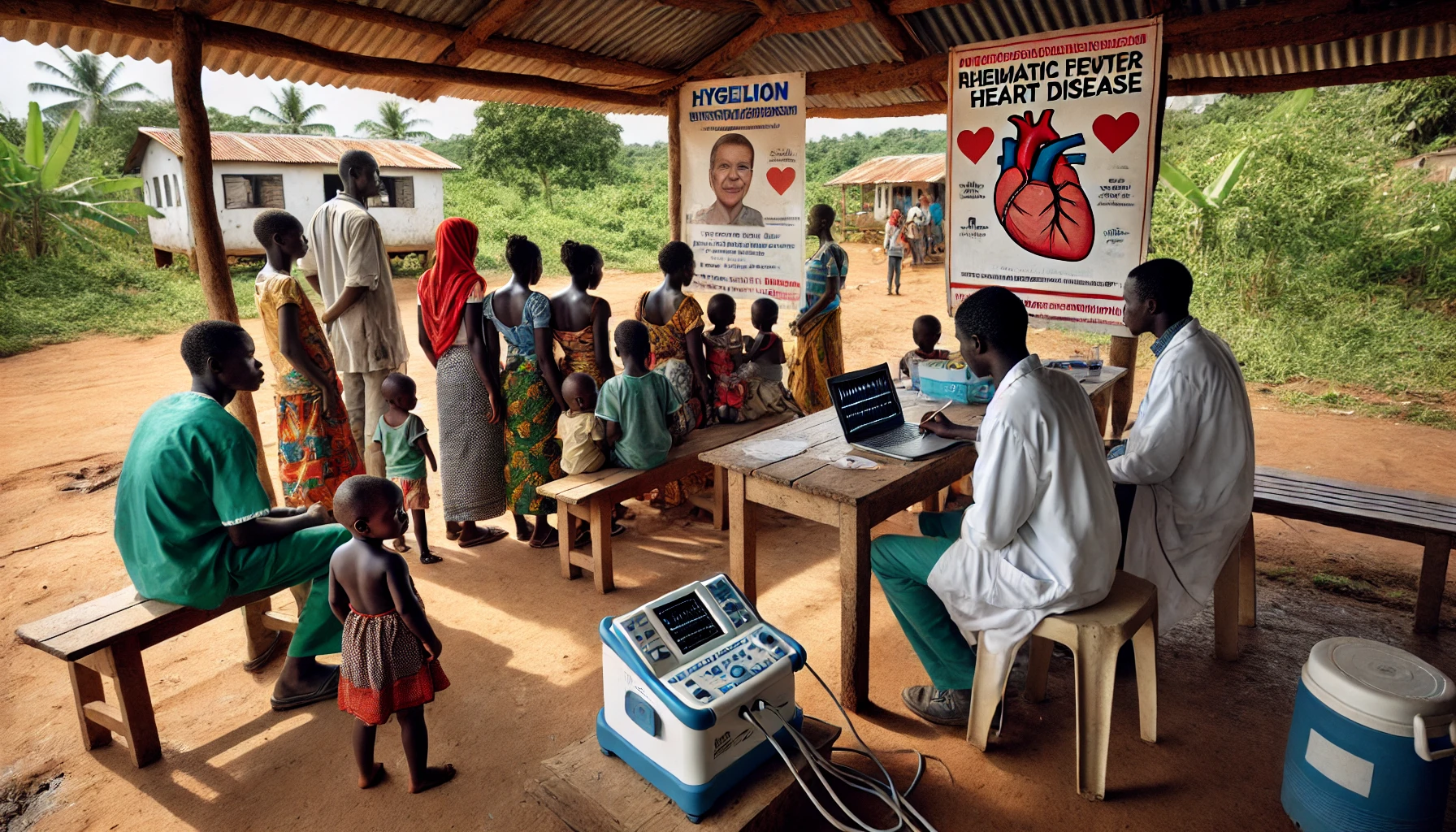
Diagnostic Tools for Early Detection
The GDG also formulated recommendations on the use of diagnostic tools for RF and RHD. In settings where echocardiography is not available, the guideline suggests the use of handheld or portable echocardiography devices to screen for RHD, particularly in high-risk populations such as pregnant women and school-aged children. This approach can facilitate early detection and improve outcomes by allowing timely interventions. The guidelines also address the need for ongoing monitoring and support for individuals receiving long-term antibiotic prophylaxis, recommending strategies to improve adherence to treatment and reduce the risk of complications such as endocarditis or heart failure.
Peer Review and Quality Assurance Process
The final guideline underwent a rigorous peer review process, with input from an External Review Group comprised of experts in RF and RHD. The role of these reviewers was to provide feedback on the technical content, ensure the clarity of the recommendations, and offer insights into the practicalities of implementation in various healthcare settings. Once peer-reviewed, the guideline was approved by WHO’s internal quality assurance team to ensure it met the highest standards of accuracy and applicability.
In summary, WHO’s guideline on the prevention and diagnosis of RF and RHD provides a robust framework for addressing these preventable diseases in high-risk populations. Through evidence-based recommendations, it emphasizes the importance of early prevention, accurate diagnosis, and long-term management strategies. The guideline aims to reduce the global burden of RF and RHD, particularly in resource-limited settings, by providing healthcare providers with clear and actionable guidance.
- READ MORE ON:
- World Health Organization
- WHO
- rheumatic heart disease
- Newborn
- RHD
- FIRST PUBLISHED IN:
- Devdiscourse
ALSO READ
"Action must be taken against the members who are using such defamatory language": Congress MP Manickam Tagore
UPDATE 1-No indication of warning before bombing of Gaza hospital, WHO says
No indication of a warning before bombing of Gaza hospital, WHO says
There is larger conspiracy, time will prove who hatched it: Congress MP Jebi Mather on cash found from Singhvi's seat
Indonesia agrees to repatriate Filipino woman who spent years on death row over drug trafficking










