New WHO Guidelines Boost Global Efforts to Prevent Tuberculosis: Key Populations and Treatments Focused
The World Health Organization (WHO) has released updated guidelines on tuberculosis preventive treatment, highlighting new strategies for high-risk populations, including people with HIV, healthcare workers, and households in contact with TB patients. This second edition report emphasizes a combination of effective screening methods, targeted testing, and modern treatment regimens, including shorter, more accessible options for treating both drug-susceptible and drug-resistant TB. With a focus on vulnerable groups like pregnant women, children, and those exposed to multidrug-resistant TB, these guidelines offer a comprehensive strategy to help eliminate TB globally.
WHO’s Updated Tuberculosis Guidelines Target High-Risk Populations
The World Health Organization (WHO) has introduced updated guidelines aimed at strengthening global tuberculosis (TB) preventive measures. Released as part of the "WHO Consolidated Guidelines on Tuberculosis: Module 1 - Prevention, Tuberculosis Preventive Treatment, Second Edition," these guidelines serve as a critical tool in reducing TB’s spread, especially among populations most vulnerable to developing active TB. The new document outlines fresh recommendations for targeted screening, testing, and the application of preventive treatment.
A New Focus on High-Risk Groups
TB continues to be one of the world’s deadliest infectious diseases, and the WHO’s renewed focus is on identifying high-risk groups for preventive treatment. Among the populations most susceptible are people living with HIV, household contacts of TB patients, healthcare workers, and individuals undergoing treatments such as dialysis or preparing for organ transplants. These groups are highlighted because of their heightened vulnerability to progressing from latent TB infection (TBI) to active TB disease.
People living with HIV are particularly at risk due to their compromised immune systems. The WHO’s guidelines recommend that these individuals receive TB preventive treatment as part of their comprehensive HIV care. Pregnant women and children who have been exposed to TB patients are also strongly advised to undergo preventive treatments, even if TB infection testing is unavailable.
Prisoners, healthcare workers, migrants from countries with a high burden of TB, and people who use drugs are other critical groups identified in the guidelines. These populations often live or work in environments that foster the rapid spread of TB, making them a priority for systematic screening and preventive treatment.
Screening and Testing: Essential Steps to Prevention
Before initiating preventive treatment, ruling out active TB disease is essential. The guidelines provide clear instructions on the use of a combination of diagnostic tools to ensure proper TB detection. Symptom-based screening remains a key element, especially in low-resource settings where access to high-tech diagnostics may be limited. However, the WHO also recommends more advanced screening techniques, such as chest radiography (CXR) and molecular diagnostic tests, depending on the patient group and available resources.
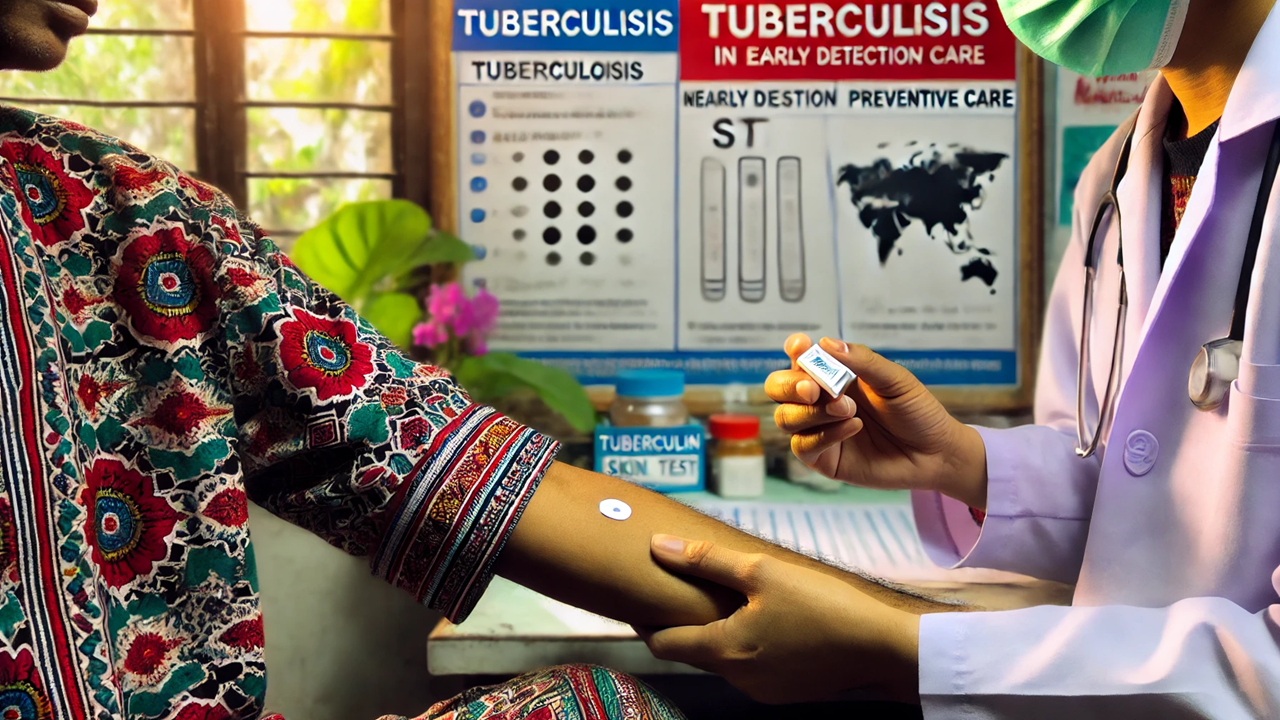
For identifying latent TB infection, WHO recommends the use of either a tuberculin skin test (TST) or an interferon-γ release assay (IGRA). The guidelines also introduce newer methods like the Mycobacterium tuberculosis antigen-based skin test (TBST), which is particularly effective in identifying infection in children and individuals with weakened immune systems.
While these tests help detect TB infection, they are not always available, particularly in low-income regions. In such cases, the WHO guidelines advise proceeding with preventive treatment based on clinical judgment, particularly for high-risk populations like people with HIV or young children exposed to TB patients.
Diverse Treatment Options, Shorter Regimens
One of the significant advancements in the new guidelines is the inclusion of diverse preventive treatment options, particularly shorter, more manageable regimens. For many years, daily isoniazid for 6 or 9 months was the standard preventive treatment. While effective, this regimen often proved difficult for patients to complete due to its length. Now, the guidelines offer alternatives such as:
3 months of weekly rifapentine plus isoniazid (3HP)
4 months of daily rifampicin
1 month of daily rifapentine plus isoniazid (1HP)
These shorter regimens have shown similar effectiveness to longer treatments but are easier for patients to follow and complete, improving treatment adherence.
For individuals exposed to multidrug-resistant or rifampicin-resistant TB (MDR/RR-TB), a six-month regimen of daily levofloxacin is recommended. This treatment is crucial for protecting individuals exposed to drug-resistant TB strains, which are harder to treat and pose a significant public health risk.
Special Considerations for Vulnerable Populations
The WHO guidelines take into account the needs of specific vulnerable populations. For instance, children, pregnant women, and people with HIV often require tailored treatment plans. Pregnant women, for example, are at higher risk for adverse outcomes if TB is contracted during pregnancy. As a result, the guidelines strongly encourage preventive treatment during pregnancy, while recommending careful monitoring for potential side effects.
Children exposed to TB, especially those under five years old, should receive preventive treatment as soon as possible if TB disease has been ruled out. Given the increased risk of rapid disease progression in young children, the WHO emphasizes the importance of timely preventive care.
In addition to providing treatment recommendations, the guidelines stress the importance of ongoing monitoring and evaluation of TB preventive programs. Countries are urged to ensure that at-risk individuals complete their treatment, which is vital for preventing the spread of the disease.
A Step Forward in the Fight to End TB
These new guidelines from the WHO represent a significant step forward in the global fight against TB. By focusing on high-risk populations and offering shorter, more accessible treatment options, the WHO aims to reduce TB transmission and bring the world closer to achieving the End TB Strategy goals. As TB remains a leading cause of death worldwide, these updated guidelines provide the roadmap necessary to protect vulnerable populations and reduce the global burden of this disease.
- FIRST PUBLISHED IN:
- Devdiscourse










