The Power of Patient Data: Improving Health Outcomes with AI and Data

Every healthcare professional, whether they’re a surgeon or a counsellor with a Masters in Mental Health, will tell you that good, clear information is absolutely paramount when providing quality healthcare. Whether diagnosing or treating a problem, doctors and nurses need access to accurate, relevant information about their patients, the conditions they may or may not be suffering from, and the treatments they have undergone or planned.
Having said all that, sometimes there’s simply too much data — too much chaff to sort the wheat out from. When researching an illness they’re trying to treat, doctors are routinely confronted with excessive volumes of reference data, research, case studies, and textbooks. Making use of this overwhelming volume of data can be difficult and intimidating. Even when simply working with one patient, there can still be so much data, information, and research that drowns out what they need to make an accurate diagnosis or assign the correct treatment.
Luckily, AI and the modern data science techniques associated with its development and use have become sufficiently advanced to aid in this process. Artificial intelligence can be used to read and summarise large volumes of research, take notes during patient appointments to allow doctors to focus on the patient, and help sort through data about the patient to figure out what information might be relevant to a diagnosis, treatment, or other factor of care.

Image Credit: National Cancer Institute on Unsplash
Different Diagnoses
When it comes to patient data, the best source of reliable information about a patient’s symptoms and other criteria that might be potentially relevant to making a diagnosis and assigning treatment, is often the patient’s electronic health record. In Australia, we have My Health Record, a centralised government database managed by the Australian Digital Health Agency that contains all details of Aussie patients’ medical histories. However it is important to note that patients do have the right to restrict certain documents from being added to their My Health Record. Centralizing health data in systems like this one allows doctors to have consistent, reliable access to a patient’s entire medical history, granting them the maximum amount of data to help them make the best judgment possible about a patient’s situation. This extensive trove of patient data can help doctors find even small details that might inform a diagnosis of a rare condition, or rule out a prescription of a common medication that the patient might happen to have an unlikely but dangerous allergy to.
But let’s be honest, a comprehensive medical history can mean a lot of data. Sorting through a patient’s entire medical history can be a massive drain on a doctor’s time, which is already in high demand. This is where AI comes in. A recent study demonstrated that ChatGPT, a publicly available generative AI tool by OpenAI, was able to diagnose patients accurately 93.3% of the time when provided with a medical history and additional information, as opposed to 76.6% accuracy with just the medical history.
Bespoke Treatments
It doesn’t stop with ChatGPT. New AI tools are being developed all the time with the specific goal of helping doctors diagnose with greater accuracy. Researchers at George Mason University have produced a new tool called MeAgainMeds.com aimed at improving the process of prescribing antidepressants. The tool helps depressed patients select the medication that is most likely to help them — while this site does not provide medical advice, it provides patients with tailored options to discuss with their healthcare team.
But AI isn’t the only new tool making waves in healthcare. In reality, AI is just one subgenre of the broader category of data science. While these AI systems appear impressive and presumably complex, in reality, the algorithms that drive them are relatively simple, especially when compared to the complex systems that run products we’re already very used to, like the Google Search algorithm. What makes AI truly useful is the massive volumes of data that the machine learning algorithms are “trained” on — they are essentially compression algorithms that represent generalised data as enormous datasets called “weights” that they call upon to determine the statistically best-fit word to come next in a sequence when outputting text responses. This makes them extremely advanced statistical analysts, but it also limits their usefulness.
Other tools, like data visualisation programs, can pick up where AI loses relevance. While AI can be good at deducing patterns given large volumes of data and generalised situations like diagnosing a medical condition, it often lacks the nuance to interpret more granular data and monitor individual situations, especially as they evolve over time. Data visualisation tools allow doctors to harness their highly trained ability to recognize patterns and situations in which certain treatments might be advantageous by making patient data easier to digest.
More accurate diagnoses, customised prescriptions, enhanced monitoring abilities — these all sound amazing and incredibly useful, but the most important question lingers: how much do they actually improve patient outcomes?
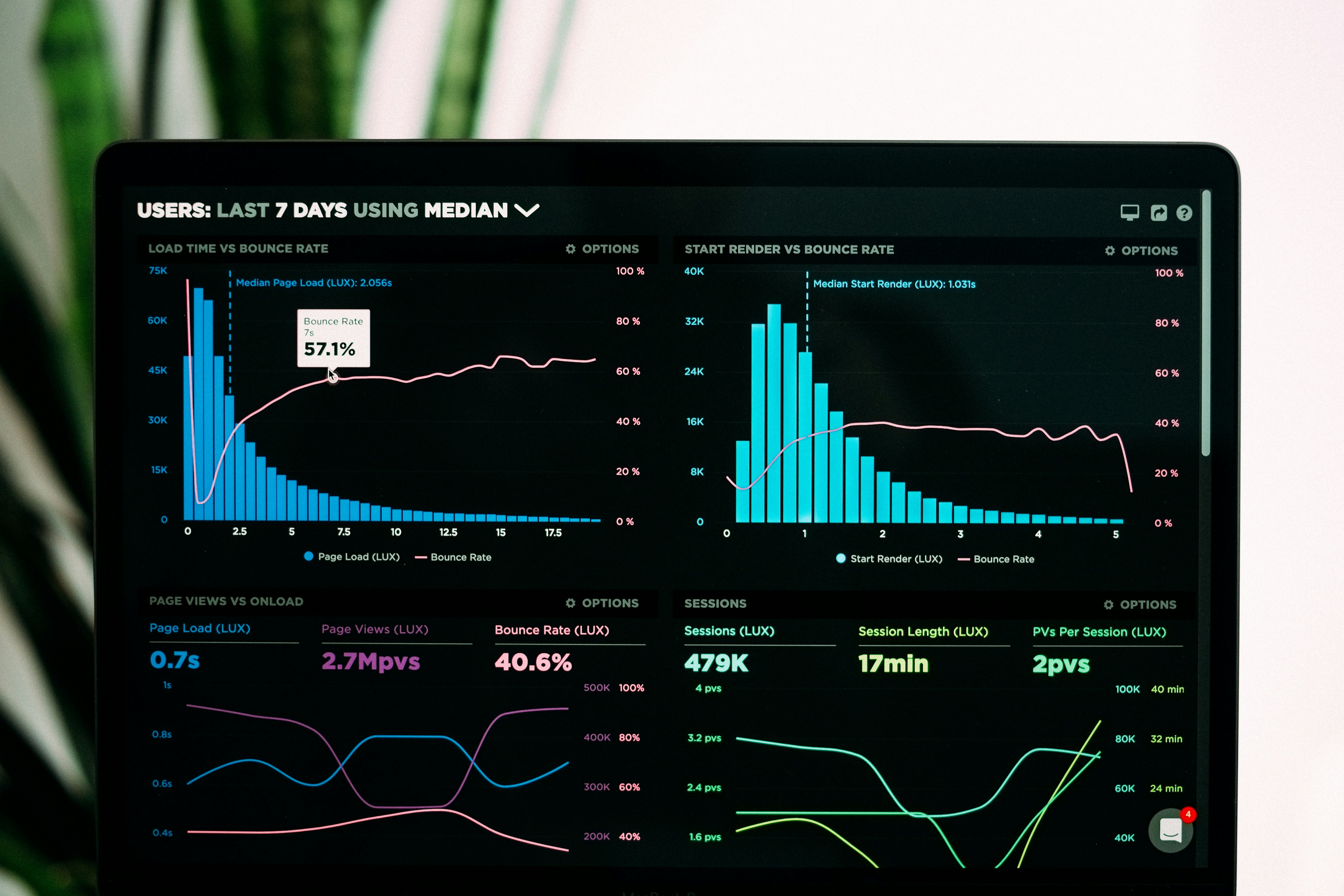
Image Credit: Luke Chesser on Unsplash
Show Me the Data
One of the best studies on the subject of AI improving patient outcomes does not, as it happens, involve any of these seemingly advanced tools used by doctors to help them perform some of their most difficult tasks. While these areas surely represent massive value and serious potential for AI to make an impact, the most comprehensive longitudinal study to date on the impact of AI systems on patient outcomes was conducted between 2016 and 2019 using an AI-driven triage system. It was found that, over the four years during which the study was conducted, patients triaged using the automated AI-based system stayed in the hospital an average of 1.3 days less. This means that the AI triage system was substantially better at properly identifying the urgency of individual patients’ needs than human nurses, and enabled patients who needed care most urgently to receive treatment faster.
These incredible tools are just the beginning. At the time of writing, the most powerful AI training cluster in the world belongs to Elon Musk’s xAI datacenter in Memphis, TN, with over 100,000 of tech giant NVIDIA’s H100 graphics processing unit (GPU) chips optimised for AI training and inference. And they aren’t even NVIDIA’s largest customer — that honour allegedly belongs to Facebook’s parent company Meta, whose founder and CEO Mark Zuckerberg recently released the world’s biggest open-source AI model to date, Llama 3.1. That means that anyone with a few GPUs at home can now run the world’s best AI. One can only imagine what incredible tools could come from these new advances, for both healthcare and the rest of the world.
(Devdiscourse's journalists were not involved in the production of this article. The facts and opinions appearing in the article do not reflect the views of Devdiscourse and Devdiscourse does not claim any responsibility for the same.)










