Opportunities and Threats in Expanding Primary Health Care through PPP in Iranian Slums
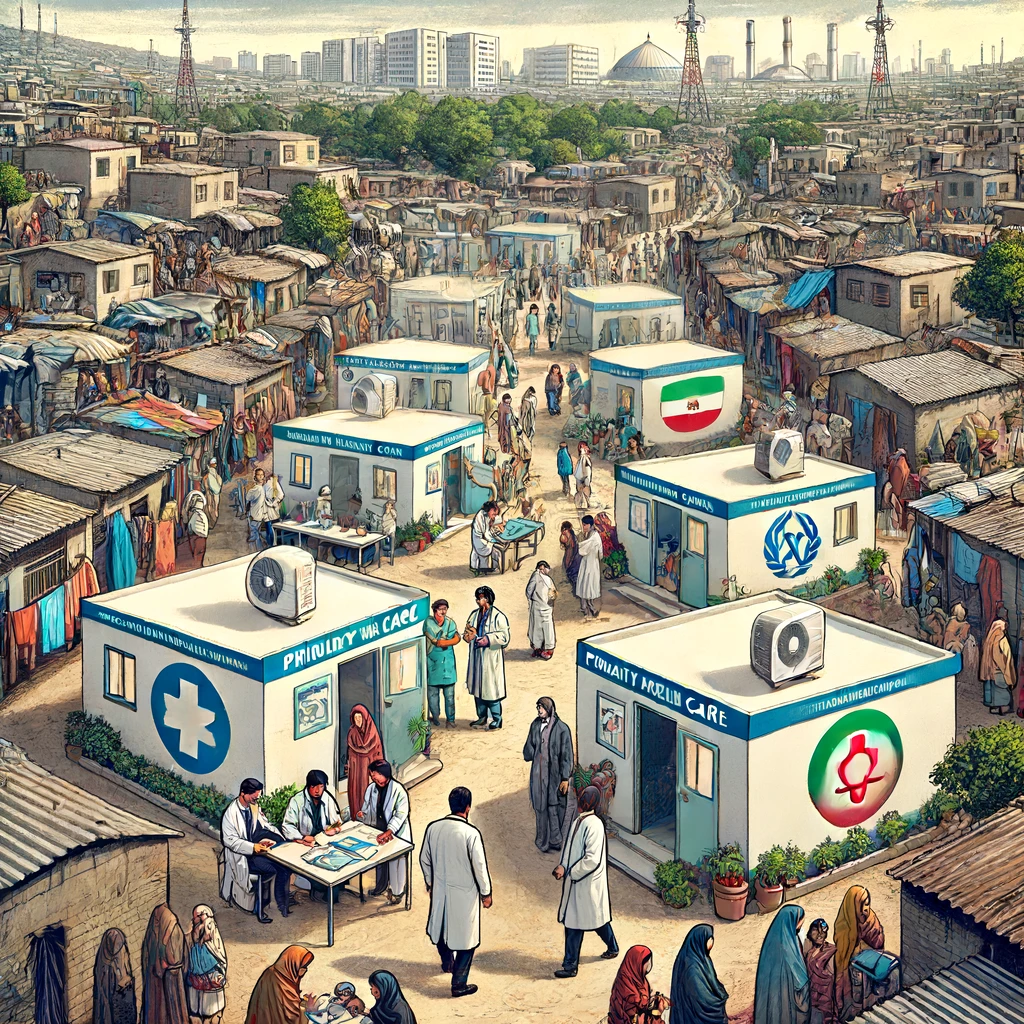
A Qualitative Study by Mashhad University of Medical Sciences, Mashhad, Iran examines how effectively primary health care (PHC) services are being expanded in slum areas of Iran through a public-private partnership (PPP) model. Conducted in 2022, this qualitative research involved interviews with 17 experts and health managers from the Khorasan Razavi province, all of whom were involved in the PHC Expansion Program. The study aims to identify the strengths, weaknesses, opportunities, and threats (SWOT) of the program based on these stakeholders' perspectives.
Effective Planning and Resource Allocation
The research highlights that addressing the economic and social determinants of health in slum settlements has become a priority for policymakers. Iran has had significant success with its Primary Health Care Program, leading to the expansion initiative using a PPP model to tackle health disparities in these underserved areas. Participants for the study were selected through purposive sampling and the snowball method. Data was gathered through semi-structured interviews held between October and December 2022 and analyzed using a five-step framework content analysis method. This process identified 23 main themes and 112 sub-themes, which were categorized into strengths, weaknesses, opportunities, and threats.
Several strengths of the PHC Expansion Program were identified. One notable strength was the thorough context analysis, which involved collecting detailed demographic and environmental data about the target population in slum areas. This data collection helped in understanding the needs and problems of the population, enabling better planning and implementation of health interventions. The development of infrastructure and physical resources was another significant strength. Before the program, there was a shortage of physical resources and standard equipment in health posts, particularly in urban slums. The program addressed this by allocating more resources, which improved the availability and quality of health services.
Challenges in Implementation and Management
The supply of human resources was also seen as a positive aspect. The program involved recruiting new healthcare workers, including doctors, midwives, nutrition experts, and psychologists, to deliver preventive services in slum areas. This helped address some of the challenges in providing these essential services. Furthermore, the expansion and strengthening of PHC services were highlighted. The program added new services such as nutrition counseling and mental healthcare, and strengthened existing services like non-communicable disease screening. This expansion increased the accessibility and equity of health services for the slum population, ensuring a fair distribution of resources according to people's needs.
However, the study also identified several weaknesses. One major issue was the outsourcing model used in the PHC program. Participants noted that the model lacked clarity and was not implemented effectively. Performance monitoring and evaluation mechanisms were also found to be inadequate, with too much focus on quantity rather than quality. Human resource management posed challenges, including job insecurity, lack of motivation, and imbalances in workload and pay. The payment mechanism was problematic, with delays in payments and an imbalance between workload and salary affecting the motivation of health workers. Additionally, the referral system was weak, with poor coordination between different levels of the health network, and project management issues were noted, including a lack of pilot phases and ineffective delegation of authority.
Leveraging Policy Support and Collaboration
The study identified several opportunities for the PHC Expansion Program. The support of policymakers and the existence of legal frameworks were seen as significant opportunities. The program received political and legal backing, which facilitated resource allocation and coordination. Inter-sectoral collaboration was another opportunity, with the involvement of various health partners and organizations helping to implement the program. The participation of the private sector was viewed as a positive aspect, with private resources being used to employ personnel and provide services. Universal health insurance coverage was also seen as an opportunity, helping to reduce health expenses for the population and facilitate access to services.
Addressing Socio-Economic and Cultural Barriers
Despite these opportunities, the study highlighted some threats to the program. Increasing urbanization and slum habitation, along with their socio-economic impacts on health, were seen as significant threats. The low capacity and experience of the private sector in providing primary health services were also noted as challenges. Additionally, the lack of coordination between service providers and insurance companies, instability of financial resources, and the cultural preference for specialists over PHC providers posed threats to the program's success.
The study underscores the importance of understanding the internal and external factors affecting the PHC Expansion Program with PPP in slum areas. This analysis provides valuable insights for health policymakers and managers to improve the performance of health facilities and address the challenges faced in these underserved areas. Future research should focus on quantitatively assessing the effectiveness of the PPP model and evaluating payment mechanisms and their impact on health outcomes and provider performance.
- FIRST PUBLISHED IN:
- Devdiscourse










